Managing Genetic Disorders: The Role of Fascia and PIASTM
Genetic disorders in children can have a profound impact on the musculoskeletal system, leading to restrictions in movement, muscle tightness, and chronic pain. The fascia, a connective tissue network within the body, plays a crucial role in maintaining structural integrity and supporting mobility. In this article, we delve into the intricate connection between fascia and genetic disorders in children, exploring how abnormalities in the fascia contribute to the manifestation of symptoms and discussing the potential benefits of PIASTM therapy by Kanu Kaushik in addressing these challenges. By examining the mechanisms underlying fascial dysfunction, as well as the therapeutic potential of PIASTM, we aim to provide valuable insights for healthcare professionals working with children affected by genetic disorders.
Introduction
Genetic disorders in children encompass a diverse range of conditions that are often characterized by impairments in physical, cognitive, and emotional development. Many of these disorders impact the musculoskeletal system, leading to mobility issues, muscle stiffness, and chronic pain. The fascia, a complex network of connective tissue that permeates the entire body, plays a pivotal role in maintaining structural integrity and facilitating movement. Abnormalities in the fascia can exacerbate the symptoms associated with genetic disorders, posing substantial challenges for affected children.
PIASTM therapy has emerged as a promising modality for addressing soft tissue restrictions and promoting tissue healing. By utilizing a specialized tool called as Accel tool designed by Kanu Kaushik to target the fascia and musculature, PIASTM therapy aims to alleviate pain, improve mobility, and enhance functional outcomes. In this article, we will explore the intricate relationship between fascia and genetic disorders in children, shedding light on the potential benefits of integrating PIASTM therapy into the comprehensive care of affected individuals.
Understanding Fascia in Genetic Disorders
Fascia, a dense connective tissue network that surrounds muscles, nerves, and organs, plays a critical role in movement, posture, and mechanical force transmission. In many genetic disorders—both common and rare—the fascia becomes structurally compromised, contributing to a range of musculoskeletal and functional problems often addressed through physiotherapy. Conditions like Ehlers-Danlos syndrome (particularly the hypermobile and classical types), Marfan syndrome, and Bethlem myopathy frequently lead to joint instability, chronic pain, and muscle weakness due to fascial laxity or fibrosis. PIASTM Therapy play a vital role in managing these symptoms through targeted interventions that aim to stabilize joints, improve posture, enhance proprioception, and reduce pain without overloading fragile connective tissues.
Rare connective tissue disorders such as Cutis Laxa, Ullrich congenital muscular dystrophy, and Pseudoxanthoma Elasticum also impact fascia, resulting in impaired movement, soft tissue weakness, or decreased elasticity. These conditions often require personalized PIASTM Therapy plans that focus on gentle strengthening, flexibility, and neuromuscular re-education to maintain mobility and prevent secondary complications like contractures or spinal deformities. Additionally, myofascial pain syndrome—a non-genetic but common comorbidity—can develop in individuals with connective tissue disorders due to abnormal fascial tension and muscle imbalances. These fascial abnormalities exacerbate the existing musculoskeletal challenges faced by children with genetic disorders, hindering their mobility and overall quality of life.
The Role of PIASTM Therapy in Addressing Fascial Dysfunction
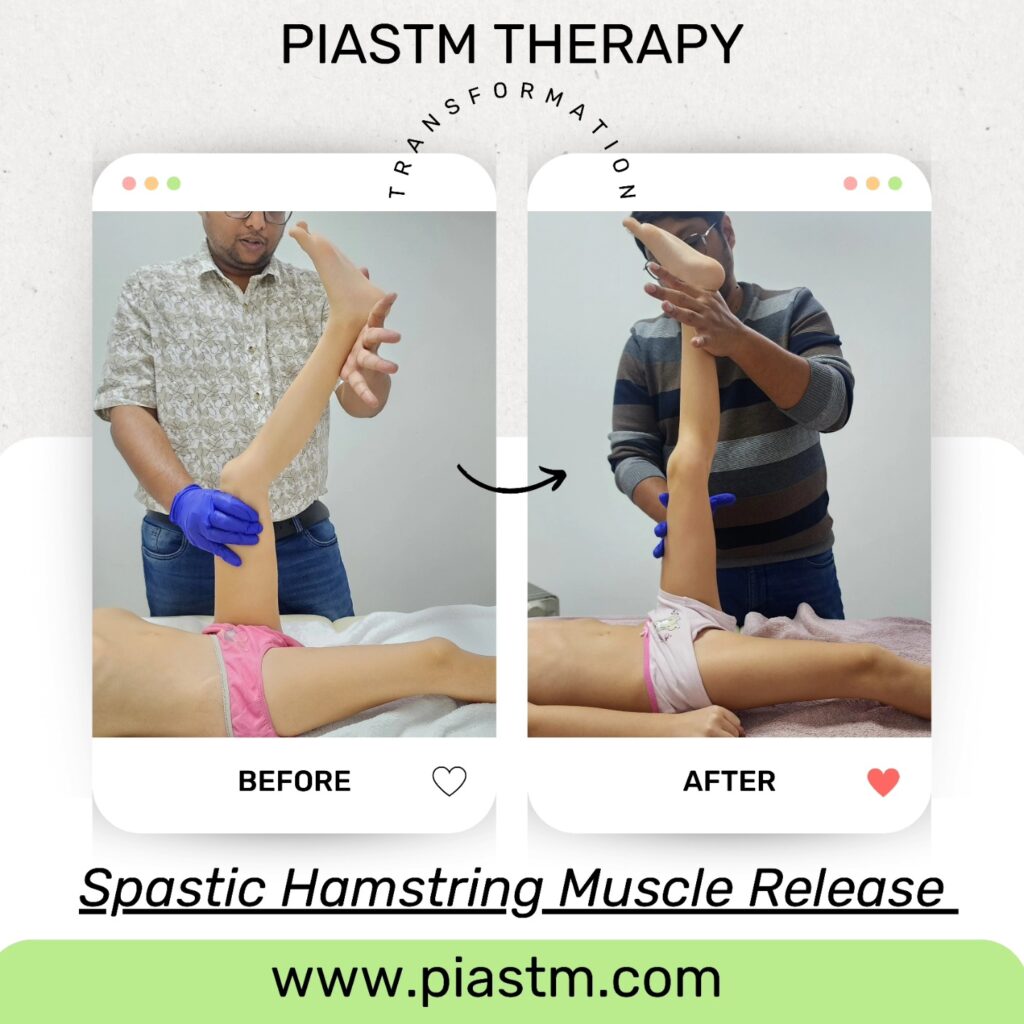
It is a specialized manual therapy technique developed by Kanu Kaushik that utilizes ergonomically designed Accel tool to detect and treat fascial restrictions, scar tissue, and myofascial adhesions. In individuals with fascial dysfunction—particularly those with genetic connective tissue disorders such as Ehlers-Danlos syndrome, Marfan syndrome, or Bethlem myopathy—PIASTM offers a controlled, low-force method to improve tissue mobility without overloading fragile structures. By targeting superficial and deep fascial layers, PIASTM can stimulate localized circulation, promote collagen remodeling, and decrease adhesions that limit range of motion or cause pain. This is particularly valuable for patients whose fascia is structurally compromised, making traditional deep-tissue approaches inappropriate or harmful.
In clinical practice, PIASTM therapy is often integrated into physiotherapy programs aimed at restoring functional movement, enhancing proprioception, and reducing chronic pain.
For patients with rare connective tissue disorders, where fascial laxity or fibrosis is a primary concern, PIASTM can help improve tissue glide and reduce compensatory muscle tension. Importantly, therapists must adapt pressure and frequency based on individual tolerance and tissue integrity to avoid microtrauma. When used alongside strengthening, postural retraining, and neuromuscular techniques, PIASTM provides a valuable tool for addressing the complex biomechanical challenges posed by fascial dysfunction, contributing to improved mobility, pain relief, and overall quality of life.
Case Study With PIASTM
Maria, a 5-year-old girl diagnosed with Ataxia-Telangiectasia (A-T)—a rare, progressive genetic disorder affecting the nervous system and muscle control—presented with mixed muscle tone characterized by alternating hypotonia (low tone) in the trunk and spasticity in the limbs. She experienced delayed motor milestones, frequent falls, postural instability, and fascial tightness along the cervical and thoracolumbar regions. Conventional physiotherapy improved her gross motor function to some extent, but her therapist noted persistent myofascial restrictions and compensatory movement patterns.
Maria was introduced to PIASTM therapy under the care of Kanu Kaushik, the founder of the technique, using the Accel PIASTM tool to gently mobilize restricted fascia and reduce localized tension. Treatment sessions were carefully adapted to her neurological status, targeting areas of increased tone while supporting flaccid muscle groups through improved fascial glide and proprioceptive input. After 4 days, Maria demonstrated improved trunk control, better balance, a reduction in limb stiffness, and increased confidence during walking and play. This case illustrates how PIASTM can be effectively tailored for children with complex genetic disorders and mixed muscle tone, offering a safe, non-invasive method to support functional gains and enhance overall quality of life.
Future Directions and Implications
As the understanding of fascial dysfunction and its impact on genetic disorders in children continues to evolve, ongoing research and clinical insights can further elucidate the potential benefits of PIASTM therapy in addressing these challenges. By exploring potential future directions for research and clinical practice, and discussing the implications of integrating PIASTM therapy into the comprehensive care of children with genetic disorders, this section can provide valuable insights for healthcare professionals and researchers dedicated to advancing the field of pediatric musculoskeletal health.
Conclusion
In conclusion, the role of fascia in genetic disorders in children is a complex and significant area of consideration for healthcare professionals. By understanding the impact of fascial dysfunction on the musculoskeletal challenges faced by affected children, and by recognizing the potential benefits of PIASTM therapy in addressing these concerns, we can take meaningful steps towards enhancing the care and quality of life of these individuals. Through continued collaborative efforts, parents can harness the therapeutic potential of PIASTM therapy to improve outcomes and support the well-being of children with genetic disorders.